In This Blog
- Overview of terminology
- What does dual diagnosis mean
- What co-occurring disorders mean
- Historical context for the terms
- Practical differences in how they’re used
- How assessment guides planning
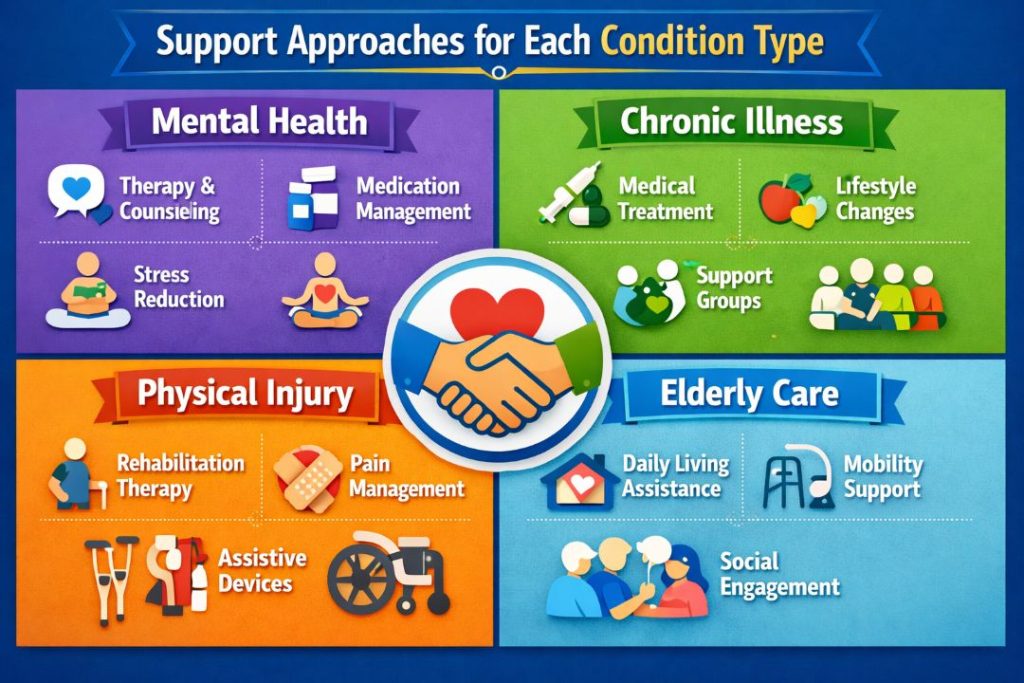
- Support approaches for each condition type
- Coordination of structured services
- Choosing appropriate support settings
“Dual diagnosis” and “co-occurring disorders” are the other names that are mostly used when talking about mental health and substance-related issues. These terms are used to identify conditions when there are two or more conditions present at the same time; however, they are also used in other cases or with a different emphasis. Knowledge of the meaning and the use of these terms would assist individuals and support networks to make informed choices regarding assessment, planning, and structured care options.
“Dual diagnosis” and “co-occurring disorders” are both terms that are used to describe combinations of conditions that could affect each other. The variations in terms do not alter the fact that each case is unique and needs to be planned individually, and it should not be assumed that some categories are fixed. Professionals make use of such terms so that they can communicate effectively regarding what an individual is experiencing and how this experience can be integrated to achieve a decision regarding integrated support.
This paper describes the definitions of each of the terms, their differences in practice, and how structured support services go about planning, assessment, and continuity of care in cases where a condition coexists with another.
What “Dual Diagnosis” Means
The term “dual diagnosis” historically refers to the presence of both a substance-related condition and another behavioral or psychological condition in the same individual. It highlights that two distinct categories of conditions are present simultaneously.
In practice, dual diagnosis is used to communicate that the assessment has identified both sets of concerns and that planning should consider how they interact. For example, an individual may experience anxiety-related challenges alongside substance use patterns that affect daily functioning. Using the term “dual diagnosis” signals the need for integrated approaches rather than treating each condition in isolation.
The emphasis in dual diagnosis is on identifying two distinct domains that require attention within a structured plan.
What “Co-Occurring Disorders” Means
The term “co-occurring disorders” is closely related and is frequently used in professional and research contexts to describe the presence of more than one condition at the same time. It is often preferred because it avoids implying a strict priority or sequencing of conditions.
Co-occurring disorders include combinations of emotional or behavioral challenges with substance-related concerns. The wording focuses on the simultaneous presence of multiple conditions without assigning one as primary and the other as secondary.
In practical terms, co-occurring disorders emphasize coordinated planning and support rather than separate streams of care.
Historical Context for the Terms
Medical, psychological, and recovery-focused fields have evolved their language over time. Dual diagnosis appeared in earlier literature to highlight the complexity of treating substance-related and other behavioral challenges together. As understanding deepened, the term “co-occurring disorders” gained prominence because it places equal emphasis on all present conditions.
While the language differs, the underlying idea is that structured services should be integrated, collaborative, and responsive to multiple needs simultaneously.
Language choice may vary by region, provider type, or professional tradition, but the goal remains aligned: clear communication that multiple conditions exist and warrant coordinated planning.
Expert Advice: Integrated assessment and planning support coordinated care for individuals with more than one condition.
Practical Differences in How the Terms Are Used
In some settings, “dual diagnosis” is used more commonly than “co-occurring disorders,” while in others the opposite is true. The difference lies mainly in emphasis rather than substance.
Term | Typical Emphasis | Common Context |
Dual Diagnosis | Substance-related + another condition | Clinical assessment contexts |
Co-Occurring Disorders | Simultaneous conditions without priority | Treatment planning and research |
Integrated Support | Coordination across needs | Recovery-oriented services |
The table helps illustrate how usage may differ without implying one term is inherently better or worse. Both describe situations where multiple conditions are present and influence structured care planning.
How Assessment Guides Planning
Assessment plays a key role in determining whether dual diagnosis or co-occurring disorders are present. A thorough evaluation considers symptoms, patterns of substance use, emotional responses, behavior changes, and how these factors affect daily functioning.
Assessments help determine:
- Whether multiple conditions are present
- How symptoms interact or influence each other
- Appropriate levels of support or supervision
- Ongoing monitoring needs
Accurate assessment supports informed decision-making rather than assumptions about diagnoses or support needs.
Support Approaches for Each Condition Type
Once assessments identify more than one condition, support planning focuses on integration rather than separation. Historically, some services treated conditions sequentially (first one, then the other). However, research and practice increasingly support coordinated approaches that consider all conditions together.
Integrated support may involve:
- Combined planning sessions
- Cross-discipline collaboration
- Coordinated monitoring of symptom changes
- Shared progress reviews
These approaches help ensure that changes in one condition are considered in relation to the other, rather than in isolation.
For integrated support planning, contact DeLand Treatment Solutions
Coordination of Structured Services
Coordinating structured services means aligning schedules and goals and monitoring strategies so that changes in one condition are communicated effectively across support providers. Rather than dividing services into separate streams, integrated coordination emphasizes continuity.
Coordination can involve:
- Regular multidisciplinary meetings
- Shared documentation when consented
- Unified progress tracking
- Adjustments based on overlapping needs
The goal is to minimize fragmentation and enhance continuity of care.
FACT: The presence of multiple simultaneous conditions is common in behavioral health and substance-related contexts.
Factors That Affect How Conditions Present Together
Multiple factors influence how co-occurring conditions or dual diagnoses manifest in individuals. These factors help professionals anticipate support needs and plan accordingly.
Common influencing factors include:
- Duration and intensity of substance use
- Emotional or stress responses
- Access to routine support systems
- Previous exposure to structured services
- Overall physical health
Understanding these factors helps tailor support rather than applying uniform approaches.
Choosing Appropriate Support Settings
Selecting a support setting when more than one condition is present involves careful consideration of structure, intensity, and coordination capacity. Not all environments are equally equipped to handle simultaneous needs.
Support Setting | Structure Level | Coordination Focus |
Moderate | Ongoing courses and check-ins | |
High | Frequent sessions, close monitoring | |
Very High | Around-the-clock support |
Selecting the setting that aligns with needs depends on assessment findings, risk considerations, and personal goals. Coordination remains central regardless of the setting.
Planning Next Steps After Assessment
After identifying dual diagnoses or co-occurring disorders, planning often includes:
- Establishing priorities for structured sessions
- Scheduling regular monitoring
- Building continuity strategies
- Identifying support networks
- Considering transition steps as progress changes
Planning evolves with participation data and informed feedback rather than fixed timelines.
For help with assessment and planning, contact DeLand Treatment Solutions
Post-assessment planning supports adjustments over time as individuals gain insight into patterns, triggers, and responses to structured support.

How Integrated Planning Supports Long-Term Progress
Integrated planning bridges initial assessment with ongoing participation. It helps individuals consolidate routines, apply coping strategies, and monitor changes in symptom patterns across conditions.
Elements of integrated planning include:
- Shared goals that reflect all conditions present
- Regular check-ins with multidisciplinary teams
- Documentation of changes and adjustments
- Feedback loops that inform ongoing decisions
This approach supports continuity rather than reactive changes when challenges arise.
Structured continuity supports informed participation and collaboration among providers and support networks.
DeLand Treatment Solutions offers coordinated support services that address dual diagnosis and co-occurring disorders through integrated planning, professional oversight, and collaborative monitoring. Programs emphasize continuity of care, structured assessment, and tailored support options designed to respect individual needs and evolving goals.
Medical Disclaimer: This blog is for informational purposes only and is not a substitute for professional medical advice.
Key Takeaways
- “Dual diagnosis” and “co-occurring disorders” both describe simultaneous conditions.
- Language differences reflect emphasis rather than fundamentally different concepts.
- Assessment guides planning and support
- Integrated coordination enhances continuity of care
- Setting selection aligns with needs, structure, and monitoring
FAQs
What is the difference between dual diagnosis and co-occurring disorders?
“Dual diagnosis” typically refers to a substance-related condition alongside another behavioral condition, whereas “co-occurring disorders” broadly describes the presence of multiple conditions at the same time. Both terms emphasize the need for integrated support, coordinated care, and planning rather than addressing each condition in isolation.
Why does terminology matter?
Terminology matters because it guides communication among professionals, supports accurate assessments, and shapes how care is planned. Clear, consistent language ensures that all providers understand an individual’s needs, helps coordinate services effectively, and allows individuals and families to comprehend the nature of conditions and the integrated support required.
How does assessment guide integrated planning?
Assessment identifies which conditions are present, how they interact, and what level of structured support is needed. Integrated planning uses these insights to design schedules, align treatment goals, and monitor progress across providers, ensuring that each condition is addressed simultaneously without gaps in care or conflicting interventions.
Can dual diagnosis and co-occurring disorders be treated separately?
Treating conditions separately can create gaps in care and reduce overall effectiveness. Integrated approaches coordinate interventions for all present conditions, improve continuity, and ensure consistency in monitoring and support. Addressing multiple needs simultaneously helps individuals achieve more stable, sustainable progress in recovery and daily functioning.
What should I ask a provider about integrated support?
Ask how services are coordinated, how goals and progress are shared across providers, and what monitoring systems track outcomes. Inquire about adjustments over time to respond to evolving needs. These questions ensure that integrated support is structured, continuous, and responsive to all co-occurring conditions present.
References
- National Institute on Drug Abuse
- Substance Abuse and Mental Health Services Administration
- Centers for Disease Control and Prevention
- National Alliance on Mental Illness
- PubMed