In This Blog
- Understanding the Baker Act and what it can’t achieve
- What voluntary mental health care is
- Who can qualify for voluntary mental health treatment alternatives
- Advantages of choosing voluntary mental health services
- Common settings providing voluntary mental health care services
- How voluntary care helps maintain long-term stability
The state of Florida has an involuntary mental health assessment in the Baker Act, which entails an assessment of an individual believed to be dangerous to themselves or other people or unable to take care of themselves as a result of mental illness. Although such law has been meant to make people feel safer, this involuntary treatment may be a terrifying, disempowering and disruptive experience to persons as well as to their families.
The programs are centred on consent, collaboration and dignity and provide structured and evidence-based mental health services. One should be able to comprehend voluntary choices before the situation grows out of control and turns into involuntary action.
Understanding the Baker Act Framework
The Baker Act refers to a Florida statute that offers an involuntary mental health assessment according to some legal requirements. It is targeting emergency cases where urgent action is deemed to be necessary.
Key features include:
- Provisional involuntary inspection.
- Legal limits are associated with the danger of safety.
- Not too long in duration unless by court order.
- Treatment based on evaluation instead of long-term treatment.
The Baker Act is not supposed to be a comprehensive therapy avenue, but more of an option as needed during an emergency.
Limitations of Involuntary Mental Health Care
The concept of involuntary admission has been given, and it does have the shortcoming of stabilising acute crises. People can become powerless, puzzled, or distrustful of providers. Such emotional reactions may disrupt participation and follow-up to therapeutic sessions upon discharge.
Common concerns include:
- Lack of personal choice
- Disturbing business and family.
- During admission, there was a disturbance of feelings.
- Limited continuity of care
These reasons highlight the need for voluntary options in which safety is allowed.
What Voluntary Mental Health Care Means
Voluntary mental psychiatric care is the kind of care that one willingly opts to join without being compelled by the law. The first one is consent, and individuals can decide to take treatment within guidelines.
Voluntary care emphasis:
- Group modality of treatment planning.
- Autonomy of clients is respected.
- Transparent communication
- Personal engagement in recovery objectives.
This practice is in line with the recovery approaches to mental health.
Who Qualifies for Voluntary Alternatives
Not all those who are afflicted with the distress of the mentality need compulsory treatment. Voluntary care is generally suitable for people who:
- Symptom awareness and support requirements.
- Not under direct threat of injury.
- Can be involved in treatment decision-making.
- Ready to participate in organised care.
Such tests can be used to determine appropriateness in voluntary admission.
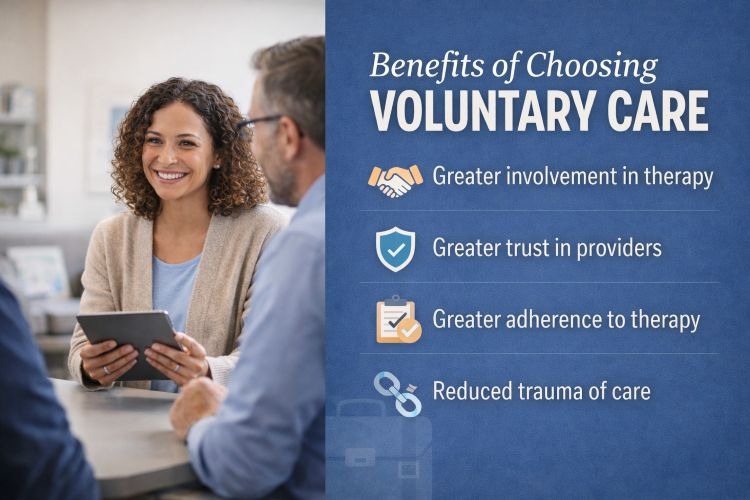
Benefits of Choosing Voluntary Care
The various benefits of voluntary mental health care are quite numerous.
These include:
- Greater involvement in therapy.
- Greater trust in providers
- Greater adherence to therapy.
- Reduced trauma of care
The scientific literature is unanimous in the idea that involvement of the client and the alliance are predictors of improved outcomes.
Speak with DeLand Treatment Solutions Professionals Today
Settings That Offer Voluntary Mental Health Care
On several levels of treatment, voluntary treatment is available, depending on needs.
Level of Care | Description |
InclientsResidential | Organised Residential Mental Health Treatment |
Partial hospitalisation | Intensive day programming and no stay-over |
Intensive Outpatient | Several instances of therapy every week |
Outpatient Therapy | Continued counselling and psychiatric treatments |
Each setting has different levels of structure and support.
Involuntary Mental Health Treatment
Voluntary incentive programs provide 24-hour support, all the while keeping consent-based Partial hospitalisation. Individuals agree to admission and treatment. Hence, the process of complete stabilisation in a controlled environment can take place.
These programs typically contain:
- Psychiatric evaluation
- Individual as well as group therapy
- Medication management as needed
- Discharge and aftercare planning
Voluntary incentives can avert an escalation to involuntary measures.
Expert Advice: “Voluntary care strengthens engagement while respecting autonomy and safety.”
Partial Hospitalisation as an Alternative
Partial hospitalisation programs are often great Baker Act alternatives. They provide intensive therapeutic services during the day, and people are allowed to return home in the evenings.
Benefits include:
- High intensity
- Maintaining routines of daily life
- Reduction in stigma compared to stigmatisation
This model is consistent with early intervention and stabilisation.
Contact DeLand Treatment Solutions for voluntary mental health support
Intensive Mental Health Care
Intensive outpatient programs feature a certain amount of structured therapy several times per week. They are good for individuals who need more than weekly therapy but do not need constant supervision.
IOPs focus on:
- Symptom management
- Coping skill development
- Emotional regulation
- Relapse prevention for mental health symptoms
They are one common step down from better levels of care.
The Role of Early Intervention
One of the most important benefits of voluntary care is early intervention. Asking for help before the symptoms get out of control may mean that emergencies where you are forced to stay in the centre are less likely.
Early intervention supports:
- Symptom stabilization
- Reduced ization risk
- Improved long-term outcomes
Voluntary care allows proactive mental health handling.
FACT: Voluntary mental health care can prevent crisis escalation when accessed early.
Autonomy and Dignity in Treatment
Voluntary mental health takes dignity and respect into consideration. Goal-setting, treatment planning, and progress evaluation are done with the individual.
This collaborative model:
- Enhances motivation
- Builds self-efficacy
- Minimises the dynamics of the adversary
Autonomy is a therapeutic asset, not a barrier
Family Involvement in Voluntary Care
With consent, families can be involved in education and support planning. Family engagement often works by providing improved understanding, communication, and continuity after discharge.
Family involvement may include:
- Psychoeducation sessions
- Family therapy
- Participation in discharge planning
Participation is inspired by appropriateness and preference.
Addressing Safety in Voluntary Settings
Safety is also a priority even in voluntary care. Programs implement monitoring, risk assessments, and crisis protocols to be able to respond to these symptoms promptly if they get worse.
Voluntary status does not imply the absence of structure and surveillance. Ethical programs are in balance with responsibility.

Transitioning From Voluntary Care
Voluntary treatment is based on continuity. Discharge planning often includes referrals for therapy in the outpatient setting, psychiatric follow-up, and support in the community.
Strong transitions equate to low relapse and rehospitalisation risks.
Common Misconceptions About Voluntary Treatment
Some feel that voluntary care is “less serious” than involuntary care. This is inaccurate. Voluntary programs can be very structured and intensive, with factors of consent being more important than any particular level of intensity or structure.
It is found that effectiveness is in virtue of appropriateness and engagement rather than legal status.
When Involuntary Care May Still Be Necessary
Voluntary care does not always work. If an individual is the immediate cause of danger to themselves or others, involuntary intervention may be necessary in the interest of safety.
Understanding voluntary options does not negate the role of emergency laws, but it helps in reducing unnecessary usage.
Choosing the Right Program
While looking for voluntary mental health care, consider:
Evaluation Factor | Why It Matters |
Licensed clinicians | Ensures professional oversight |
Evidence-based therapy | Supports effectiveness |
Clear admission criteria | Indicates ethical practice |
Aftercare planning | Promotes continuity |
Informed choices improve outcomes.
Ethical Considerations in Mental Health Care
Ethical mental health treatment prioritises the least restrictive environment when appropriate. Voluntary care conforms to this principle as it stands by the concept of safety, yet upholds the concept of autonomy.
This approach is founded on modern standards of mental health practice.
Choosing DeLand Treatment Solutions mental health care, people can access structured, professional support without having to be traumatised by being involuntarily admitted. When treatment is entered into voluntarily, people are often more involved, motivated, and open to long-term planning for care. Ethical programs put dignity first when providing sound mental health services.
Medical Disclaimer: This blog is for informational purposes only and is not a substitute for professional medical advice.
Key Takeaways
- The Baker Act is meant for emergencies, not ongoing care.
- The emphasis of voluntary mental health treatment is based on consent and cooperation.
- Early voluntary care can help in curbing the risk of involuntaryization.
- Multiple levels of voluntary treatment provide flexibility of choices.
- Autonomy and dignity foster therapeutic engagement.
- Ethical programs strike a balance between safety and the least restrictive care.
FAQs
What is a Baker Act alternative option?
A Baker Act alternative refers to voluntary mental health care options that individuals choose without legal compulsion. These programs provide structured, evidence-based treatment while preserving autonomy and consent. They are appropriate when someone is not an immediate danger and can participate in care decisions.
Who qualifies for voluntary mental health care?
Individuals who recognise their symptoms, are not at immediate risk of harming themselves or others, and are willing to engage in treatment typically qualify for voluntary care. An assessment determines appropriateness, ensuring safety while respecting autonomy and treatment readiness.
Is voluntary treatment as effective as involuntary care?
Voluntary treatment can be equally effective or more effective when it is appropriate. Engagement, trust, and collaboration often improve outcomes. Effectiveness depends on symptom severity, level of care, and follow-through, not whether treatment is voluntary or involuntary.
Can voluntary care prevent Baker Act admission?
Yes, early voluntary treatment can reduce the likelihood of crisis escalation that leads to involuntary admission. Addressing symptoms proactively through structured care often stabilises individuals before emergency thresholds are reached, supporting safety and continuity.
What levels of voluntary mental health care exist?
Voluntary care includes inpatient residential treatment, partial hospitalisation, intensive programs, and standard outpatient therapy. Each level provides different intensity and structure, allowing treatment to match needs while maintaining client consent.
What happens if symptoms worsen during voluntary care?
If symptoms worsen, clinicians reassess safety and treatment needs. Programs have protocols for increased monitoring, higher levels of care, or emergency intervention if necessary. Voluntary status does not remove responsibility for safety and ethical decision-making.